You’ve probably heard of psoriasis—the chronic inflammatory condition that can cause itchy, scaly patches on your skin. Less well-known is a rare form of the disease called pustular psoriasis, which affects roughly 1% of people with psoriasis1.
Pustular psoriasis is characterized by pustules, or small pus-filled bumps that can be incredibly painful2. Not surprisingly, they can severely affect your quality of life, especially if the pustules are located on areas that need to withstand pressure, like the soles of your feet, or on highly visible skin, like your face. This condition might be uncommon, but it’s important to distinguish pustular psoriasis symptoms from an infection because it can be easy to mistake the two. Here’s everything you need to know about pustular psoriasis, including the symptoms, causes, and treatment.
What is pustular psoriasis? | What causes pustular psoriasis? | Pustular psoriasis types | Pustular psoriasis treatments | What makes pustular psoriasis worse?
What is pustular psoriasis?
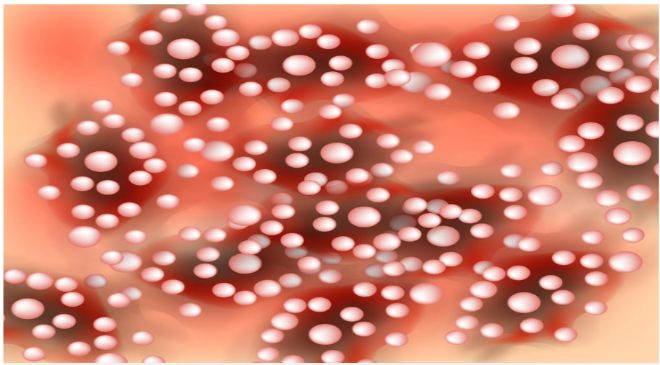
Pustular psoriasis is a rare type of psoriasis that similarly goes through periods of flare-ups and remissions. During a flare-up of pustular psoriasis, the inflamed skin will be covered with small bumps filled with pus, or pustules. These bumps may spread, join together, and break open, according to the American Academy of Dermatology (AAD).
It’s important to note that pustular psoriasis isn’t just a skin condition. “It’s a multisystem3 inflammatory disorder,” Dawn Davis, MD, a pediatric and adult dermatologist at Mayo Clinic, tells SELF. “A lot of people assume that when you get psoriasis it’s limited to the skin only, but we’re understanding more and more that it really is a disease that is multi-organ and manifests more obviously in the skin.”
This means that the chronic inflammation associated with pustular psoriasis can affect other areas of your body as well. What’s more, there’s increasing research indicating that all forms of psoriasis are associated with a variety of diseases that involve chronic inflammation such as inflammatory bowel disease, arthritis, and even cardiovascular diseases4. However, there’s no evidence that pustular psoriasis causes other inflammatory diseases—researchers are still trying to understand the connection.
What causes pustular psoriasis?
Experts don’t know the exact cause, but they do know pustular psoriasis is the result of an overactive immune system that attacks healthy cells in your body, according to the Centers for Disease Control and Prevention (CDC). The fluid that fills the pustules consists of white blood cells, which are immune cells that the body normally sends to fight infection5.
Although the causes of pustular psoriasis remain a mystery, experts have honed in on a few risk factors for the condition. Research shows that pustular psoriasis is associated with genetic mutations of the CARD14 gene, which helps regulate genes responsible for the immune system, according to the NLM. People with these mutations may be susceptible to developing the condition, which can be triggered by a particular event, such as an infection, smoking, or pregnancy6.
Quitting certain medications—oral corticosteroids, in particular—is another common trigger of pustular psoriasis, Lawrence Green, MD, a board-certified dermatologist and clinical professor of dermatology at George Washington School of Medicine and member of the American Academy of Dermatologists board of directors, tells SELF. Oral corticosteroids are commonly prescribed to treat plaque psoriasis, and your immune system can have an adverse reaction when you finish a course of medication7. This is why people commonly have both plaque psoriasis and pustular psoriasis.
Getting diagnosed with pustular psoriasis can be tricky. It can be hard to tell at first glance (even for your doctor) whether the pus is a sign of infection or psoriasis. The only way to confirm is to take a culture of the pus to find out whether there are bacteria inside. If it is pustular psoriasis, then the bacterial culture will be negative, because pustular psoriasis is not caused by an infection and therefore, not contagious. Another option is for your doctor to take a biopsy of your skin to be examined under the microscope.
Back to top
What are the different types of pustular psoriasis and their symptoms?
All pustular psoriasis is characterized by fluid-filled pustules. To start, you may develop tender, reddened skin followed by pustules that generally pop up a few hours after your initial symptoms, according to the Mayo Clinic. “A lot of people suspect these bumps are an infection when actually it’s not,” Dr. Davis says.
Oftentimes, the pustules merge and then burst open8, resulting in a scaly, cracked, and painful rash. More pustules can form, and the cycle repeats, according to the AAD. Flares may last up to months without pustular psoriasis treatment.
The different types of pustular psoriasis are defined by the area of the body where the pustules appear.
Palmoplantar pustular psoriasis
As the name suggests, palmoplantar pustular psoriasis commonly affects the palms of the hands as well as the soles of the feet. The pustules often develop in sweat ducts6, which are more densely packed on the palms and soles than anywhere else on the body. As with other types of pustular psoriasis, the skin typically becomes irritated and inflamed before breaking out in pustules. A scaly plaque usually forms several days after the pustules form, according to the
National Organization for Rare Disorders (NORD). You may have a burning sensation in your hands and feet that make it hard to stand or touch anything.
The exact causes of palmoplantar pustular psoriasis are unknown, but researchers suspect smoking may be a risk factor since many people with the condition have a history of smoking. Experts suspect that smoking may inflame the sweat glands and cause pustules to form, according to NORD. People assigned female at birth are more likely to have this condition than people assigned male at birth, though researchers aren’t sure why.
Generalized pustular psoriasis (GPP)
This type causes pustules to cover your entire body and comes with symptoms such as a fever, chills, and fatigue. It’s a dangerous condition that requires urgent medical care to reduce inflammation, according to the AAD. Over time, this chronic inflammation can lead to serious complications like liver damage or heart failure.
GPP is often triggered by starting or stopping certain medications, viral infections, and pregnancy, according to the National Library of Medicine (NLM), though the exact trigger is usually unknown.
Pustular psoriasis of pregnancy (PPP)
In some cases, pregnancy triggers pustular psoriasis, potentially because of fluctuating hormone levels. Typically, PPP occurs at the beginning of the third trimester of pregnancy and clears up after childbirth. Usually, the pustules form under the breasts or around the armpits before spreading to other parts of the body. Early detection and treatment are really important because PPP can be dangerous to the fetus and the person who is pregnant9. Unfortunately, if you have PPP during pregnancy, your risk for flare-ups during subsequent pregnancies increases.
Acropustulosis of infancy
Even babies and young children can develop pustular psoriasis. Pustules form on the palms of the hands and soles of the feet, and it’s not clear why they develop. Some researchers theorize that acropustulosis of infancy could be triggered by scabies, which is a super itchy condition caused by a mite10. Although the condition can chronically flare up for years, it often disappears by age three11.
Back to top
What are some pustular psoriasis treatments?
For localized flare-ups, topical treatments such as steroids or retinoids, which is a derivative of vitamin A, are generally used first. Both can help bring down inflammation, and they are sometimes prescribed together, according to the AAD. Additionally, Dr. Davis recommends taking warm baths with Epsom salt or colloidal oatmeal (ground oatmeal), both of which can reduce inflammation and itching. Add whichever you prefer to a warm—not hot—bath, and soak for 15 minutes, the Mayo Clinic recommends.
For more severe flare-ups, you’ll need systemic medications. According to Dr. Green, your dermatologist will usually recommend immunosuppressive medications that suppress the body’s overall immune response, like cyclosporine or methotrexate. These drugs aren’t targeted, so they suppress your entire immune system, making you more susceptible to infections. That’s why a newer type of medication, known as biologics, can be highly effective for pustular psoriasis treatment. Because they only target specific parts of the immune response, biologics are less likely to cause unwanted side effects, Dr. Davis says.
Biologics are designed to target specific aspects of the immune response. Most of the biologics used for psoriasis target a part of the immune response called interleukins 12, 17, and 23, which are inflammatory cells secreted by white blood cells during a flare-up of plaque psoriasis. However, newer research shows that these are not the main immune response involved in pustular psoriasis. Another inflammatory cell called cytokine 36 is the main one that’s overexpressed in pustular psoriasis, Dr. Green explains. Clinical trials are currently in progress to develop biologics specifically targeting that specific cell.
What makes pustular psoriasis worse?
Stress is a huge pustular psoriasis trigger, according to Dr. Davis. “Medical, physical, or emotional stress makes psoriasis worse,” she says. Any lifestyle changes that reduce your overall level of stress can also reduce your risk of a psoriasis flare-up.
Of course, avoiding stress isn’t always possible—and if you have pustular psoriasis, the condition itself can be a source of stress, which may create a painful cycle. “It’s difficult to have such an impactful skin disease,” Dr. Davis says. “Psoriasis patients have a higher incidence of mental health concerns12, and they express concerns about work truancy, school truancy, and being treated differently by peers. It really impacts your quality of life,” she says. This is especially true if your psoriasis shows up on a highly visible area of your body. “If you have palmar psoriasis and you shake people’s hands for a living, or you have facial psoriasis and you’re on camera for a living, that can be very difficult,” Dr. Davis says.
The good news is that remission (meaning your symptoms are virtually gone or very minimal) of pustular psoriasis is possible with proper treatment. If you suspect you have pustular psoriasis, schedule an appointment with a board-certified dermatologist, who can diagnose you and come up with an effective treatment plan. “Don’t assume it’s an infection, especially if you have plaque psoriasis,” Dr. Green advises.